Anthrax puts fear into cattle producers and with good reason.
Cattle are very susceptible along with a long list of other species, including bison and horses. It is also considered a zoonosis which means humans can contract it.
Fortunately, it is generally the cutaneous (skin) form in humans and responds well to antibiotics. Unfortunately, terrorist groups have used anthrax spores as a form of bioterrorism. (This is not new — it was used in the First World War to infect horses.) Humans only very rarely get the fatal inhalation form. In fact, in 2006, with the hundreds of producers and veterinarians exposed to anthrax only two contracted the skin form and were treated.
Read Also
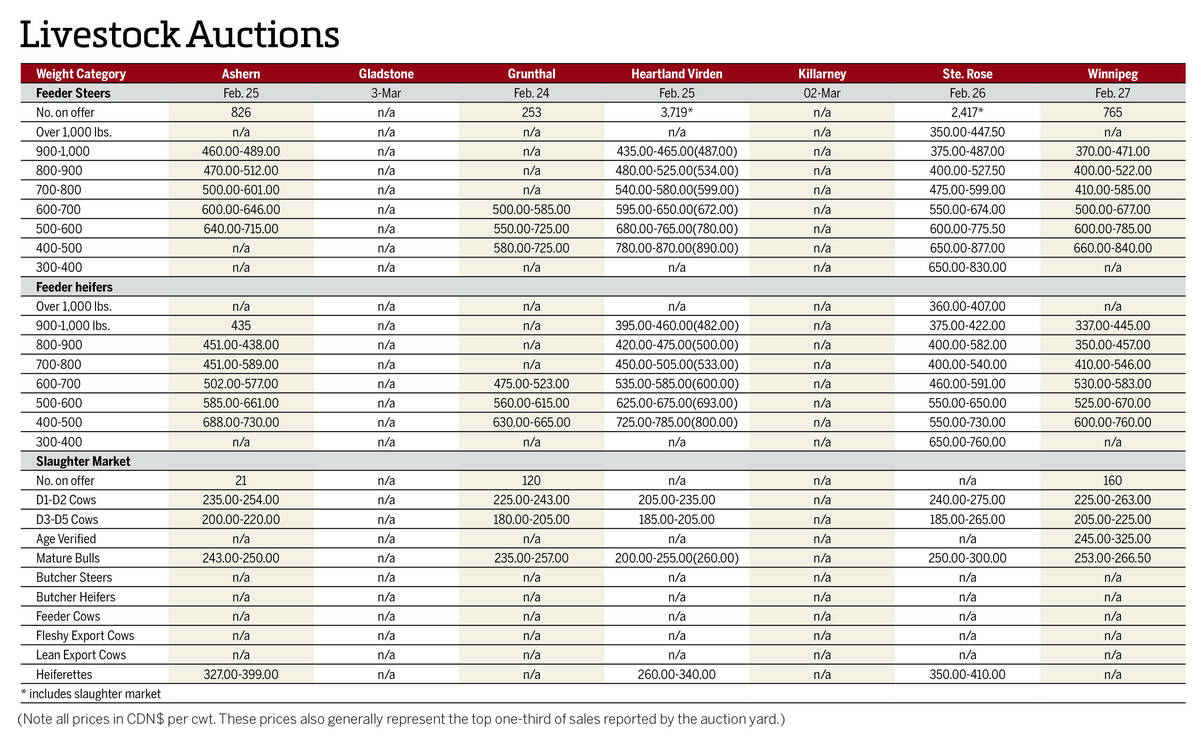
Manitoba cattle prices, March 4
Chart of weekly Manitoba cattle prices.
Anthrax has killed cattle and bison in several outbreaks over the last 100 years, but the biggest was in Saskatchewan and Manitoba in 2006, when more than 800 animals died on over 150 different premises. Approximately 20 to 25 outbreaks have been reported in cattle across Canada since 1967.
Cattle, bison, horses, moose, deer, and other species contract the spores from the soil and spores can remain infective for at least 250 years if deeply buried. Soils high in organic material and calcium and with a higher pH make survival more likely, while spores on the soil surface break down in a few years.
Outbreaks occur primarily in wet springs followed by a very hot, dry summer or in very dry conditions. Very wet springs bring the spores to the surface, while in dry years, livestock generally will graze low areas close to the ground where they normally don’t have access and contact the spores.
If enough spores are ingested, a toxemia results in very sudden death. Toxemia results in severe weakness and co-ordination depression followed quickly by death. All sudden deaths in cattle should be autopsied by your herd veterinarian. Not only do they qualify for the BSE program, finding out the cause of anthrax in the sentinel case allows you and your neighbours to initiate a preventive program. Based on blood not clotting, lack of rigor mortis to the carcass, and other findings such as an enlarged spleen, anthrax may be diagnosed or at least suspected on the original post-mortem.
Ideally, if suspected, the carcass should not be opened. The diagnosis can be made from collecting a few drops of blood. There are many causes of sudden death, so in most cases the carcass will be completely opened up before anthrax is suspected.
The problem is often that it is not the first disease your veterinarian will suspect. Lab backup is required to confirm it. Spraying with formaldehyde to prevent scavenging by predators initially, and burying with lye are also accepted procedures. Until complete disposal has taken place, take care to keep dogs, cats and humans away from the carcass.
The Canadian Food Inspection Agency used to help with disposal and decontamination, but no longer compensates producers to help offset losses and disposal costs. It still is reportable to both the federal and provincial authorities, but the labs do that automatically if there is a positive confirmation.
The preventive vaccine is a non-encapsulated live spore vaccine (sterne 32F4 strain). It is called the anthrax spore vaccine and is manufactured by a Colorado serum company. Immunity to the vaccine is almost 100 per cent with two shots three to four weeks apart. These must be boostered yearly in order to maintain immunity, preferably just before summer, the prime time for contraction. At $2 to $3, the cost is comparable to other cattle vaccines. It’s administered subcutaneously and slaughter withdrawal in cattle would be around 42 days. It is only available from one distributor in Canada and most veterinarians don’t normally stock it.
It becomes a decision between the producer and his veterinarian as to how long to continue. My recommendations would be to vaccinate if a herd of cattle or bison were diagnosed in your immediate area, especially if on the same water course. In the 2006 Saskatchewan outbreak, CFIA veterinarian Dr. Greg Douglas recommended vaccinating all cattle, horses, sheep, goats and bison within a five-mile radius of all positive cases. This is very wise advice.
Vaccinating cattle for anthrax is not part of most routine preventive programs because the incidence is very low and sporadic. However, since the spores are extremely resistant, if cattle were pastured in areas with a history of anthrax, I would vaccinate indefinitely. Cost is minimal and protection is high.
If there has never been a case in your immediate area, there is probably no need to vaccinate. But there have been reported incidences of anthrax coming in on the feed. This is easily possible where round bales are made in old lake bottoms in a drought and dirt gets wound into the bales. If sourcing feed from a confirmed anthrax area, this would be another good reason to vaccinate. The cost of valuable purebreds may make the decision to vaccinate easier.
If diagnosed, the best plan is to move cattle as quickly as possible off the contaminated pasture or area and either vaccinate or first treat with long-acting penicillin, wait eight days, and then vaccinate. The vaccine is very susceptible and rendered ineffective by antibiotics if they are given simultaneously.
You and your herd veterinarian will weigh the pros and cons of each method. This may depend on how quickly it was diagnosed and the handling facilities available. With bison, this is difficult as it is generally at a time when the calves are still small. Commonly the bulls are disproportionately affected as they are often in the breeding season and more stressed than the cows.
Discussion should occur with your regular veterinarian on their vaccination protocols. He or she would be familiar with the past history of anthrax in your area and could best advise you. It is extremely important to have all cattle sudden deaths autopsied so the first case is not missed. Vaccination will provide some protection as soon as seven days with total protection by 14 days after administration.
An outbreak back in 1991 in four Alberta locations was thought to be linked to migratory birds from Wood Buffalo Park — a theory that has some credibility. Our practice diagnosed one of those outbreaks and vaccinated for four years after the then-mandatory two years (for a total of six years). Vaccination was then stopped at the owners’ request and the herd has not had another case since. But had it been my choice, I would have kept vaccinating.
The vaccine is labelled for cattle, so we vaccinate bison extra label. Because the vaccine technically has a shorter level of immunity (roughly six months), we try to vaccinate when just going out to pasture. The problem with bison is they are just going to start calving. Dr. Dave Hunter, who is chief bison veterinarian for Ted Turner Enterprises, has done some interesting work with doubling the dose, which seems to extend immunity. He recently double dosed using a needleless vaccinator and got an even greater immune response. Withdrawal, of course, will be longer. But this may shed some light on getting better and longer protection and more easily allows us to fit this into our management programs with other vaccines. We don’t know yet how long this method may protect our vaccinated animals.
Fortunately, anthrax can be controlled well with vaccination, and unfortunately we have to live with it cropping up every so often in the three western provinces — often in new locations. It is also prevalent in the Midwest U.S., especially in some areas of Texas.
Discuss all vaccination requirements with your herd veterinarian, as this summer saw a few outbreaks across the Prairies because of the hot, dry summer. Just like vaccinating for the clostridial diseases, vaccinating for anthrax is a no-brainer if endemic in your area.